Want to Reduce Your Risk of Death? Fitness Matters More Than Weight Says a New Study
It’s long been clear that, for most people, long-term obesity places them at greater risk of developing conditions such as diabetes and heart disease that not only reduce their quality of life but increases the risk of premature death.
But losing substantial amounts of weight by restricting what you eat can represent an enormous challenge. Can you protect your health and life by increasing physical activity instead? Might it make sense, in other words, to be “fat but fit”?
Many studies have investigated this central question, and an exhaustive new review of them has reached an unequivocal answer: in their paper, published last month in the journal iScience1, Glen Gaesser and Siddhartha Angadi report that the health risks associated with being obese can be reduced or even abolished by moderate-to-high levels of physical activity and cardiorespiratory fitness – even while weight remains the same. Weight loss by itself, they say, is not consistently associated with a lower risk of mortality.
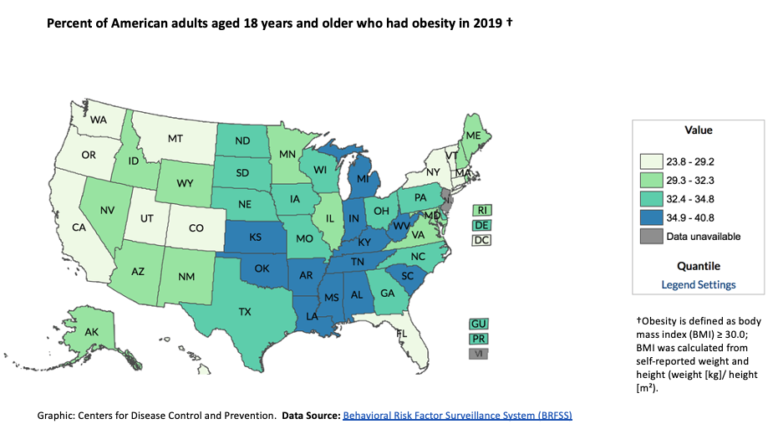
Rates of obesity were already nearing 4 out of 10 people in many central and southern states in 2019; at the current rate of growth 50% of Americans are predicted to be obese.
As rates of obesity have climbed – and are predicted to include 50% of American adults by the year 20302 – life-shortening and life-limiting illnesses associated with being obese, such as diabetes, hypertension, and cardiovascular, liver and kidney disease have risen in their wake.
Many studies have compared the effect of physical activity, or losing weight by restricting calories, on the biological markers for these diseases – indicators such as the blood levels of glucose and fat, responsiveness to insulin and blood pressure. The findings and statistics for many of these studies have since been amalgamated by reviews called “meta-analyses”, pooling the results for many thousands of people in the search for a common theme. It’s largely from a comprehensive survey of these that Gaesser and Angadi have drawn their conclusion.
It has been shown that significant reduction in weight can improve or even reverse diseases such as diabetes and hypertension3. But losing weight by eating less and, more importantly, keeping it off, is hard – even the relatively modest 5% of weight4 sufficient for a significant improvement in the biological markers that indicate a person’s health status. The body becomes accustomed to a higher BMI and evolution has conditioned it to treat attempts to reduce weight as starvation, reacting by sharply increasing the sensation of hunger and by reducing metabolism to burn fuel more efficiently. That painful reality has heightened interest in whether there might be another way.
Becoming fitter reduces your risks – even if you remain obese
Gaesser and Angadi conclude that increasing cardiorespiratory fitness or even just physical activity improves these cardiometabolic markers at least as much as weight loss does alone. When it comes to the risk of mortality, they say fitness is likely to be more protective than losing weight.
The review finds that increasing physical activity is associated with a reduction in death from any cause of between 15% and 50%, and an only slightly smaller improvement in the risk of death from cardiovascular disease.
The studies included in Gaesser and Angadi’s review measured cardiometabolic fitness either in terms of METs (multiples of the energy used by a person at rest), or by each 1 ml of oxygen used per kg of bodyweight per minute (1ml/kg/min). Most of them then define the state of being “fit” fairly modestly, ruling anyone except the least fit 20 – 25% of participants into this healthier category. Moving from an unfit or low fitness status to a higher category is associated with lower all-cause mortality of between 30% and 60%. There was also a “dose-dependent” effect of fitness: each one-MET increase in cardiorespiratory fitness was associated with a reduction in mortality from any cause of 14% to 29%.
How is “fitness” measured?
Cardiorespiratory fitness itself is measured according to a concept known as VO2 Max – the amount of oxygen a person consumes when they are working as hard as they can during a maximal exercise test. It’s expressed as milliliters of oxygen, per kilogram of bodyweight, per minute of exercise.
A person at rest is conventionally considered to be using around 3.5ml/kg/min of oxygen – a metabolic rate known as 1 MET. If he or she doubles that consumption during exercise (this would be a slow walk) he or she is said to be using 2 metabolic equivalents or 2 METs.
Interestingly, 1 MET – also thought of as the basal metabolic rate (BMR) – uses about 1 kcal/kg/hr, so that a 75kg person uses around 75 calories simply in maintaining this resting metabolism. Some of the studies cited in the Cell review used “time to exhaustion” to measure fitness, which correlates very well, if not perfectly, with the more precise MET-based measurements.

Fitness can be assessed by using a mask to measure the amount of oxygen used by a person exercising at maximum effort.
It’s the level of fitness that matters

The fitter you are the more you reduce the risks of dying from being overweight or obese. If you’re unfit, then even being a normal weight won’t protect you from risk.
The review investigated the effect of exercise on the risk of death from cardiovascular disease as well as mortality in general, and found that moving from an unfit or low fitness category to a fit one was associated with a reduction in this risk of almost half5 and an even bigger decrease in the risk of stroke6.
Once again there was a dose-dependent relationship between fitness and risk: one study found that each 1 MET improvement in fitness was associated with an almost 20% lower risk of death from cardiovascular disease7, and another showed that each 1ml/kg/min increase in fitness was associated with a 15% reduction in this risk8.
One of the review’s key messages is about the danger of being unfit, whether you’re obese or not. It concludes that unfit people, even if they are of normal weight, are in significantly greater danger both of dying prematurely of any cause or of dying as a result of conditions such as diabetes or cardiovascular disease than fit people who are overweight or obese. The message is not only that increased fitness can be used as a way of countering the hazards of being obese, but that fitness is essential in its own right to avoiding these life-shortening and disabling diseases.
Attempting to lose weight “isn’t working” for most people – it could be making things worse
Gaesser and Angadi look at several aspects of weight loss to cast doubt on its effectiveness as the main tool in tackling the diseases associated with obesity.
Their main objection is the poor record of weight loss programs – using either dieting or increased exercise – in reducing BMI. They suggest that the roughly threefold increase in obesity in the United States since the late 1970s9 at the same time as the attempts to lose weight have spread further through the population of the United States10 shows that weight loss has been ineffective as a tool to confront cardiometabolic disease.
Multiple failed attempts at a healthier BMI have led to successive reductions and increases in weight tending to ratchet it upwards. This cycling of weight appears to increase the risk of sarcopenic obesity11 in which generally health improving muscle is lost during dieting and replaced with fat during relapses, a condition associated with a 24% higher risk of all-cause mortality12.
Gaesser and Angadi suggest that some of the illness and death associated with obesity could be a result of weight variations. They cite a number of studies indicating the danger of this cycling – especially to older and more overweight people – including a 41% increased risk of all-cause mortality and 36% higher risk of death from cardiovascular disease13. One study of patients on statins found that the fifth whose weight varied most faced an almost doubled risk of heart attack and stroke14.
The review points out that simply losing fat – for example through liposuction – is no guarantee of a reduced risk of disease15. Bariatric surgery – restricting the size of the stomach and bypassing sections of intestine – often sees a dramatic improvement in cardiometabolic risk factors. However, these improvements come before a significant reduction in bodily fat can take place to account for them.
Exercise targets the most dangerous fat
It’s become clear in recent years that fat is so metabolically active that it can be regarded as a hormonal organ. Indeed, it is often the source of damaging background inflammation in the bodies of obese people, as well as releasing unwanted fat molecules into the blood, and disrupting the normal uptake and use of glucose. As Gaesser and Angadi point out, the fat stored in some regions of the body – such as around the main organs – poses a much bigger threat to health than that stored elsewhere, subcutaneously for example. Fat that invades the pancreas can damage the ability to make insulin. Fat accumulating in the liver might account for only about 1% of the body’s total store16, but given the liver’s central role in managing the burning of food for fuel it can wreak havoc.
But exercise appears to target this fat in particular. Weight loss resulting from exercise is associated with a 50% greater loss of visceral fat than the same weight reduced through caloric restriction17. The Cell review cites meta-analyses which found that exercise reduced visceral fat significantly with relatively little loss of body weight (often less than a kilo)18, 19, 20. Other studies found the particularly dangerous fat in the liver particularly susceptible to exercise, even when there was hardly any overall reduction in weight21.
Reductions in body weight have a disproportionately great effect on this abdominal store of fat. However, if a weight loss of 5% is caused by exercise training it will reduce visceral fat by 21%, whereas the same weight lost by eating less reduces it only by 13%. Gaesser and Angadi conclude that if your aim is to shed this amount of visceral fat, instead of dieting to reduce body weight by 5% you need reduce it only by 2-3% using exercise. They suggest that given that the sort of exercise used in most of the studies were in line with official recommendations, it might be easier for people to sustain than a substantial reduction in calories.
Exercise can make fat fitter too
Part of the overall system-wide effect of exercise – its “polypill” quality – is that it can make even fat cells “fitter”, with benefit for the body as a whole. The review cites studies showing that physical activity causes white fat cells to grow more mitochondria – their tiny energy generating structures – and to improve molecular signaling systems inside the cells making them more responsive to insulin22. This helps the body to process glucose healthily and to minimize the leaking of fat into the bloodstream, avoiding diseases such as diabetes.
Despite Gaesser and Angadi’s findings, substantial and sustained weight loss brought about through calorie restriction has also been shown to reduce insulin resistance3, and even to reverse diabetes (see BOX 2: “How a low calorie diet reversed diabetes”). However, Gaesser and Angadi say weight loss is no better at reducing the risk for diabetes or cardiovascular disease than exercise programs that have no weight loss target, and in some cases has been shown to have no benefit23. Given the difficulty in achieving significant weight loss, they say, exercise is a more realistic strategy for creating a similar effect.
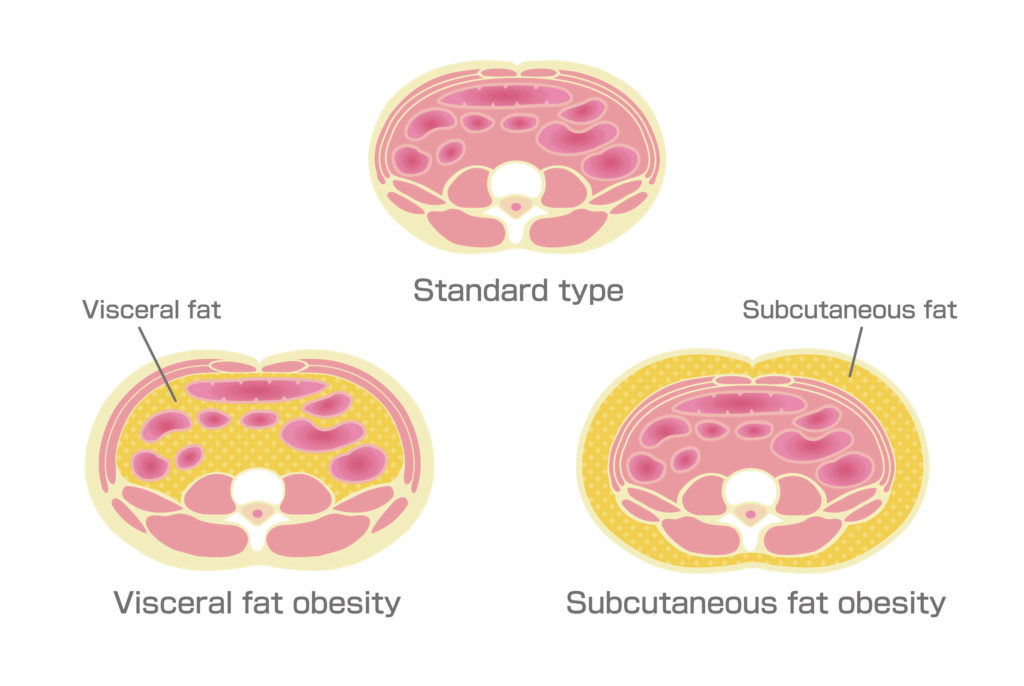
Fat stored around abdominal organs, infiltrating the pancreas and liver, is particularly dangerous to health. But exercise reduces visceral fat more quickly than more benign fat stored under the skin.
How a low calorie diet reversed diabetes.
A landmark trial carried out by scientists at Glasgow and Newcastle Universities in the UK showed that weight loss alone could reverse Type 2 diabetes – although the reduction in weight was considerable. The DiRECT trial recruited 298 National Health Service patients, and placed half of them on a diet of around 850 calories a day for three to five months followed by a careful reintroduction of “normal” food and long-term support, but had no requirement for exercise.
The study found that overall, almost half of the patients saw their diabetes go into remission within a year, such that they were able to stop taking medication for the disease. Weight loss was “dose-dependent”: 85% of patients losing 15kg (33 pounds), 57% of those losing 10-15kg (22-33 pounds) and 34% of those who lost 5-10kg (11-22 pounds) achieved remission of their diabetes.
One of the lead scientists, Professor Roy Taylor of Newcastle University said weight loss had its effect partly by reducing fat in the liver and pancreas of participants who went on the low-calorie diet allowing them to return to normal functioning. The half of patients in the control group received standard diabetes care from their General Practitioner (primary care doctor) and only 4% of them experienced remission of the disease.
But is it the exercise, or the weight loss it causes, that’s improving health?
An obvious question is whether the lower risk of mortality associated with exercise and fitness is actually caused by the weight loss that comes with it. Gasser and Angadi say it isn’t likely – partly on the basis of studies showing that physical activity usually fails to create significant weight loss24. They also cite a Norwegian study that compared unfit people who improved their cardiorespiratory fitness with those who did not. Even those who became so much fitter that they achieved a 34% lower risk of mortality and 60% lower risk of stroke, kept the same BMI as those who remained unfit25.
An interesting possible reason for improvements in health with relatively little change in weight was suggested by a study in which Danish adults achieved a 22% reduction in the risk of mortality during the 10-13 year period after they took up cycling26. It was shown that although these improvements were not associated with weight loss, there was a reduction in the cyclists’ visceral fat27.

Danes who took up cycling reduced their risk of dying by 22%. Although they lost relatively little weight, they did reduce their visceral fat.
Another result of exercise that appears to benefit health independently of weight loss is its effect on muscle quality. Muscular fitness, measured by how hard a person can perform a hand-grip, or the strength they show in knee-extensions, is associated with a lower risk of dying28, although it doesn’t match the effect of cardiorespiratory fitness. One study in which participants’ BMI, waist circumference and percent body fat were all recorded showed muscular fitness was associated with a lower risk of death independently of weight loss, even after discounting the improvement in cardiorespiratory fitness that went with improved muscles29.
In recommending that people deal with overweight and obesity principally by using exercise to again fitness Gaesser and Angadi accept that tolerating continuing obesity comes with added risk. But they insist that the fit-but-fat model, known as metabolically healthy overweight, is a more realistic goal for obese people otherwise faced with the challenge of returning to a normal BMI. Their argument is that although people who are overweight but healthy are still shown by studies be more at risk of mortality than healthy peers of normal weight, this risk disappears when cardiometabolic fitness is included in the statistics.
They also insist that improved fitness is a practical option, citing a study that showed that after only two months of moderate-intensity exercise training (or high-intensity interval training) obese adults could improve their cardiorespiratory fitness by 1 MET, which as we have seen is associated with a 14-29% reduction in mortality, and 19% lower risk of death as a result of cardiovascular disease.
The challenge that a substantial increase in even moderate exercise would pose to many overweight and obese people should not be underestimated, but the prospect of losing enough weight to achieve the same result would be daunting indeed. It is often said that you can’t outrun a bad diet, but running could go a long way to mitigating its worst effects.
- Gaesser and Angadi, Obesity treatment: Weight loss versus increasing fitness and physical activity for reducing health risks, iScience (2021), https://doi.org/10.1016/j.isci.2021.102995
https://www.cell.com/action/showPdf?pii=S2589-0042%2821%2900963-9 - Ward, Z.J., Bleich, S.N., Cradock, A.L., Barrett, J.L., Giles, C.M., Flax, C., Long, M.W., and Gortmaker, S.L. (2019). Projected U.S. State-level prevalence of adult obesity and severe obesity. N. Engl. J. Med. 381, 2440–2450.
- Lean, M.E.J., Leslie, W.S., Barnes, A.C., Brosnahan, N., Thom,G., McCombie, L., Peters, C., Zhyzhneuskaya, S., Al-Mrabeh, A., Hollingsworth, K.G., Rodrigues, A.M., Rehackova, L., Adamson, A.J., Sniehotta, F.F., Mathers, J.C., Ross, H.M., McIlvenna, Y., Welsh, P., Kean, S., Ford, I., McConnachie, A., Messow, C.M., Sattar, N. & Taylor, R. (2019). Durability of a primary care-led weight-management intervention for remission of type 2 diabetes: 2-year results of the DiRECT open-label, cluster-randomised trial. Lancet Diabetes Endocrinol. 2019 May;7(5):344-355. doi: 10.1016/S2213-8587(19)30068-3. Epub 2019 Mar 6. PMID: 30852132.
- Magkos, F., Fraterrigo, G.,Yoshino, J., Luecking, C., Kirbach, K., Kelly, S.C., de las Fuentes, L., He, S., Okunade, A.L., Patterson, B.W. & Klein, S. (2016). Effects of Moderate and Subsequent Progressive Weight Loss on Metabolic Function and Adipose Tissue Biology in Humans with Obesity. Cell Metabolism, Volume 23, Issue 4, 2016. Pages 591-601. ISSN 1550-4131, https://doi.org/10.1016/j.cmet.2016.02.005.
- Blair, S.N., Kohl, H.W., 3rd, Barlow, C.E., Paffenbarger, R.S., Jr., Gibbons, L.W., and Macera, C.A. (1995). Changes in physical fitness and all-cause mortality. A prospective study of healthy and unhealthy men. JAMA 273, 1093– 1098.
- Prestgaard, E., Mariampillai, J., Engeseth, K., Erikssen, J., Bodegard, J., Liestol, K., Gjesdal, K., Kjeldsen, S., Grundvold, I., and Berge, E. (2019). Change in cardiorespiratory fitness and risk of stroke and death. Stroke 50, 155–161.
- Lee, D.C., Sui, X., Artero, E.G., Lee, I.M., Church, T.S., McAuley, P.A., Stanford, F.C., Kohl, H.W., 3rd, and Blair, S.N. (2011). Long-term effects of changes in cardiorespiratory fitness and body mass index on all-cause and cardiovascular disease mortality in men: the Aerobics Center Longitudinal Study. Circulation 124, 2483–2490.
- Imboden, M.T., Harber, M.P., Whaley, M.H., Finch, W.H., Bishop, D.L., Fleenor, B.S., and Kaminsky, L.A. (2019b). The association between the change in directly measured cardiorespiratory fitness across time and mortality risk. Prog. Cardiovasc. Dis. 62, 157–162.
- Hruby, A., and Hu, F.B. (2015). The epidemiology of obesity: a big picture. Pharmacoeconomics 33, 673–689.
- Martin, C.B., Herrick, K.A., Sarafrazi, N., and Ogden, C.L. (2018). Attempts to lose weight among adults in the United States, 2013-2016. NCHS Data Brief, 1–8.
- Rossi, A.P., Rubele, S., Calugi, S., Caliari, C., Pedelini, F., Soave, F., Chignola, E., Vittoria Bazzani, P., Mazzali, G., Dalle Grave, R., and Zamboni, M. (2019). Weight cycling as a risk factor for low muscle mass and strength in a population of males and females with obesity. Obesity (Silver Spring) 27, 1068–1075.
- Tian, S., and Xu, Y. (2016). Association of sarcopenic obesity with the risk of all-cause mortality: a meta-analysis of prospective cohort studies. Geriatr. Gerontol. Int. 16, 155–166.
- Zou, H., Yin, P., Liu, L., Liu, W., Zhang, Z., Yang, Y., Li, W., Zong, Q., and Yu, X. (2019). Body-weight fluctuation was associated with increased risk for cardiovascular disease, all-cause and cardiovascular mortality: a systematic review and meta-analysis. Front Endocrinol. (Lausanne) 10, 728.
- Bangalore, S., Fayyad, R., Demicco, D.A., Colhoun, H.M., and Waters, D.D. (2018). Body weight variability and cardiovascular outcomes patients with type 2 diabetes mellitus. Circ. Cardiovasc. Qual. Outcomes 11, e004724.
- Seretis, K., Goulis, D.G., Koliakos, G., and Demiri, E. (2015a). The effects of abdominal lipectomy in metabolic syndrome components and insulin sensitivity in females: a systematic review and meta-analysis. Metabolism 64, 1640–1649.
- Fabbrini, E., Magkos, F., Mohammed, B.S., Pietka, T., Abumrad, N.A., Patterson, B.W., Okunade, A., and Klein, S. (2009). Intrahepatic fat, not visceral fat, is linked with metabolic complications of obesity. Proc. Natl. Acad. Sci. U S A 106, 15430–15435.
- Verheggen, R.J., Maessen, M.F., Green, D.J., Hermus, A.R., Hopman, M.T., and Thijssen, D.H. (2016). A systematic review and meta-analysis on the effects of exercise training versus hypocaloric diet: distinct effects on body weight and visceral adipose tissue. Obes. Rev. 17, 664–690.
- Keating, S.E., George, J., and Johnson, N.A. (2015a). The benefits of exercise for patients with non-alcoholic fatty liver disease. Expert Rev. Gastroenterol. Hepatol. 9, 1247–1250.
- Keating, S.E., Hackett, D.A., George, J., and Johnson, N.A. (2012). Exercise and non-alcoholic fatty liver disease: a systematic review and meta- analysis. J. Hepatol. 57, 157–166.
- Keating, S.E., Hackett, D.A., Parker, H.M., O’Connor, H.T., Gerofi, J.A., Sainsbury, A., Baker, M.K., Chuter, V.H., Caterson, I.D., George, J., and Johnson, N.A. (2015b). Effect of aerobic exercise training dose on liver fat and visceral adiposity. J. Hepatol. 63, 174–182.
- Hens, W., Taeyman, J., Cornelis, J., Gielen, J., Van Gaal, L., and Vissers, D. (2016). The effect of lifestyle interventions on excess ectopic fat deposition measured by noninvasive techniques in overweight and obese adults: a systematic review and meta-analysis. J. Phys. Act Health 13, 671–694.
- Dewal, R.S., and Stanford, K.I. (2019). Effects of exercise on brown and beige adipocytes. Biochim. Biophys. Acta Mol. Cell Biol Lipids 1864, 71–78.
- Ma, C., Avenell, A., Bolland, M., Hudson, J., Stewart, F., Robertson, C., Sharma, P., Fraser, C., and Maclennan, G. (2017). Effects of weight loss interventions for adults who are obese on mortality, cardiovascular disease, and cancer: systematic review and meta-analysis. BMJ 359, j4849.
- Foright, R.M., Presby, D.M., Sherk, V.D., Kahn, D., Checkley, L.A., Giles, E.D., Bergouignan, A., Higgins, J.A., Jackman, M.R., Hill, J.O., and Maclean, P.S. (2018). Is regular exercise an effective strategy for weight loss maintenance? Physiol. Behav. 188, 86–93.
- Ostergaard, L., Jensen, M.K., Overvad, K., Tjonneland, A., and Grontved, A. (2018). Associations between changes in cycling and all- cause mortality risk. Am. J. Prev. Med. 55, 615–623.
- Prestgaard, E., Mariampillai, J., Engeseth, K., Erikssen, J., Bodegard, J., Liestol, K., Gjesdal, K., Kjeldsen, S., Grundvold, I., and Berge, E. (2019). Change in cardiorespiratory fitness and risk of stroke and death. Stroke 50, 155–161.
- Rasmussen, M.G., Overvad, K., Tjonneland, A., Jensen, M.K., Ostergaard, L., and Grontved, A. (2018). Changes in cycling and incidence of overweight and obesity among Danish men and women. Med. Sci. Sports Exerc. 50, 1413–1421.
- Garcia-Hermoso, A., Cavero-Redondo, I., Ramirez-Velez, R., Ruiz, J.R., Ortega, F.B., Lee, D.C., and Martinez-Vizcaino, V. (2018). Muscular strength as a predictor of all-cause mortality in an apparently healthy population: a systematic review and meta-analysis of data from approximately 2 million men and women. Arch. Phys. Med. Rehabil. 99, 2100–2113.e5.
- Ruiz, J.R., Sui, X., Lobelo, F., Morrow, J.R., Jr., Jackson, A.W., Sjostrom, M., and Blair, S.N. (2008). Association between muscular strength and mortality in men: prospective cohort study. BMJ 337, a439.


